- Home
- About Cancer
- Managing side effects
- Lymphoedema
- About lymphoedema
About lymphoedema
Lymphoedema is swelling (oedema) that develops when lymph fluid builds up in the tissues under the skin or sometimes deeper in the abdomen (belly) and chest areas.
Learn more about:
- What is lymphoedema?
- The lymphatic system
- When does lymphoedema develop?
- What are the risk factors?
- How common is lymphoedema?
What is lymphoedema?
Lymphoedema occurs when the lymphatic system is not working properly. It usually occurs in an arm or leg, but can also affect other parts of the body, such as the neck.
Learn about the lymphatic system.
Lymphoedema can be either primary (when the lymphatic system has not developed properly) or secondary (when the lymphatic system is damaged). This fact sheet is only about secondary lymphoedema following treatment for cancer.
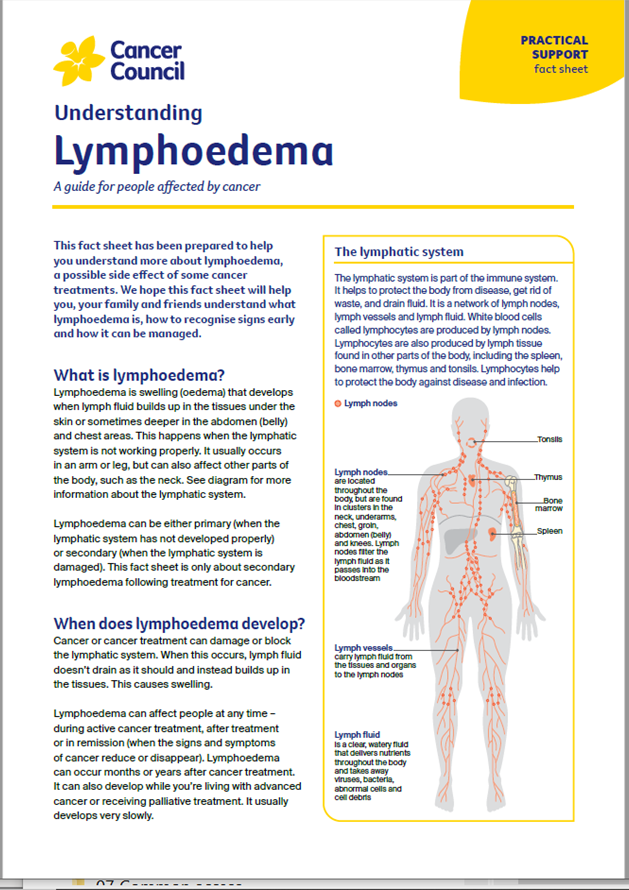
The lymphatic system
The lymphatic system is part of the immune system. It helps to protect the body from disease, get rid of waste, and drain fluid. It is a network of lymph nodes, lymph vessels and lymph fluid.
White blood cells called lymphocytes are produced by lymph nodes. Lymphocytes are also produced by lymph tissue found in other parts of the body, including the spleen, bone marrow, thymus and tonsils. Lymphocytes help to protect the body against disease and infection.
The lymphatic system consists of:
| Lymph vessels | a large network of thin tubes found throughout the body. Lymph vessels carry lymph fluid from the tissues and organs to the lymph nodes. |
| Lymph fluid | a clear, watery fluid that delivers nutrients throughout the body and takes away viruses, bacteria, abnormal cells and cell debris. |
| Lymph nodes | are located throughout body, but are found in clusters in the neck, underarms, chest, groin, abdomen (belly) and knees. Lymph nodes filter the lymph fluid as it passes into the bloodstream. |
The lymphatic system

When does lymphoedema develop?
Cancer or cancer treatment can damage or block the lymphatic system. When this occurs, lymph fluid doesn’t drain as it should and instead builds up in the tissues. This causes swelling.
Lymphoedema can affect people at any time – during active cancer treatment, after treatment or in remission (when the signs and symptoms of cancer reduce or disappear). Lymphoedema can occur months or years after cancer treatment. It can also develop while you’re living with advanced cancer or receiving palliative treatment. It usually develops very slowly.
What are the risk factors?
Whether or not you develop lymphoedema after treatment for cancer depends on the location of the cancer, its stage and the type of treatment. While the risk is ongoing, most people who are at risk never develop lymphoedema.
Some risk factors for lymphoedema include:
- surgery to remove lymph nodes – the more nodes removed, the greater the risk
- radiation therapy
- taxane-based chemotherapy drugs
- an infection in the at-risk limb
- carrying extra body weight (overweight or obesity)
- injury to the lymphatic system (e.g. a tumour growing near a lymph node or vessel)
- underlying primary lymphoedema
- inflammatory disorders such as arthritis
- not being able to move around easily.
Learn ways to reduce your risk of lymphoedema.
How common is lymphoedema?
Lymphoedema can occur after treatment for many different cancers (see below). There are few statistics about how common lymphoedema is after cancer treatment, and the incidence differs for each cancer type. One study estimated that lymphoedema occurs in about 20% of people treated for cancers of the vulva, vagina, ovary, uterus, cervix, breast, prostate, or melanoma.
Cancer type |
Commonly affected areas |
| bladder | genitals, legs |
| breast | arm, hand, breast, chest, trunk |
| cervical | genitals, legs |
| head and neck | face, below chin and/or neck |
| melanoma | any part of the body, depending on the area affected by melanoma |
| ovarian | genitals, abdomen/trunk, legs |
| prostate | genitals, abdomen/trunk, legs |
| uterine | genitals, abdomen/trunk, legs |
| vulvar or vaginal | genitals, abdomen/trunk, legs |
→ READ MORE: Early signs of lymphoedema
More resources
A/Prof Louise Koelmeyer, Director, Australian Lymphoedema Education, Research and Treatment (ALERT) Program, and Associate Professor, Macquarie University, NSW; Prof John Boyages AM, Founding Director and Honorary Professor at the ALERT Program, Macquarie University, NSW; Dr Nicola Fearn, Occupational Therapist and Accredited Lymphoedema Therapist, The Lymphoedema Clinic Wollongong, and Senior Research Officer, St Vincent’s Hospital Sydney, NSW; Jennifer Gilbert, Clinical Nurse Consultant – Lymphoedema, Icon Cancer Centre, Chermside, QLD; Megan Howard, Senior Physiotherapist and Lymphoedema Physiotherapist, Peter MacCallum Cancer Centre, VIC; Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA; Dr Amanda Pigott, Clinical Specialist Occupational Therapy, Princess Alexandra Hospital, QLD; Prof Neil Piller, Director, Lymphoedema Clinical Research Unit, College of Medicine and Public Health, Flinders University, SA, and Patron, Lymphoedema Association of Australia; Ashlynne Pointon, Consumer; Dr Cathie Poliness, Breast Surgeon, Peter MacCallum Cancer Centre, VIC; Tara Redemski, Senior Physiotherapist – Cancer and Blood Disorders, Gold Coast University Hospital, QLD.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.