- Home
- Head and neck cancers
- Managing side effects
- Swallowing difficulties
- Using a feeding tube
Using a feeding tube
As a result of surgery or radiation therapy, you may find eating and swallowing uncomfortable or difficult. A feeding tube may be inserted either before, during, or after your surgery or radiation therapy to help you get the nutrition you need. This tube is usually temporary, but sometimes it is permanent.
Learn more about:
How feeding tubes are used
A feeding tube can help ensure you maintain your weight and energy. It is important to avoid losing a lot of weight during treatment and to have enough kilojoules and fluids. If you can’t swallow medicines, check with your doctor, nurse or pharmacist whether these can also be given through the feeding tube.
Your health care team will explain how to:
- care for the tube to prevent it leaking or becoming blocked
- avoid infections – this may include washing your hands before using the tube, and keeping the tube and your skin dry
- monitor for signs that the tube needs to be replaced
- handle issues such as what to do if the tube falls out – while this is very rare it is important to let your treatment team know immediately if this happens
- ensure the tape is secure, especially after a shower – if it’s not secure, the tube can be accidentally bumped out of place.
If you have a feeding tube, it is still important to brush your teeth and keep your mouth clean even though you are not eating or drinking.
The thought of having a feeding tube can be frightening, and it is common to have a lot of questions. Getting used to a feeding tube takes time. Talking to a dietitian or nurse can help, and a psychologist or counsellor can provide emotional support and suggest ways to cope.
Types of feeding tubes
Temporary feeding tube
A thin tube is put into a nostril, then down the throat and oesophagus into the stomach. This is called a nasogastric or NG tube. It is mostly used if you need a feeding tube for a short time (e.g. the days or weeks after surgery when you can’t eat).
A doctor may put in an NG tube during an operation when you are asleep. Or a nurse or doctor may put in or remove the NG tube while you’re awake. A spray is usually used to numb the area to make it less uncomfortable to insert the tube. You will be given specially prepared liquid nutrition through this tube.

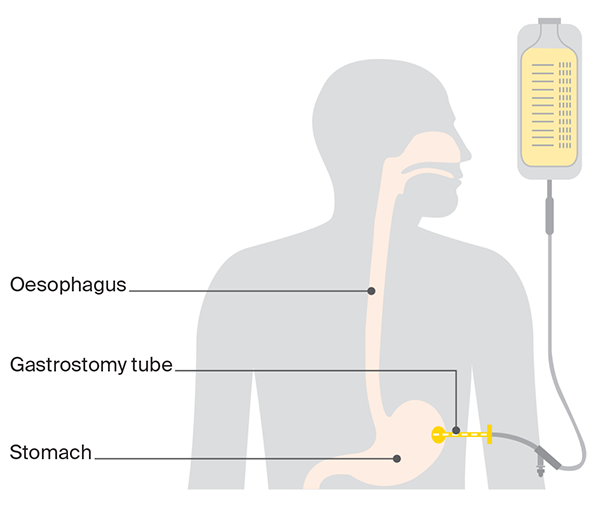
Long-term or permanent feeding tube
A tube is inserted through a hole in your belly into the stomach. This is called a gastrostomy tube. It may be used if you need a feeding tube for a longer time, such as during a recovery period from radiation therapy or after a very big operation.
Depending on the way the tube is inserted, it may be done while you’re awake or under anaesthetic. The tube may be inserted by endoscope (percutaneous endoscopic gastrostomy or PEG tube), using an x-ray (radiologically inserted gastrostomy or RIG tube), or surgically (surgical gastrostomy).
→ READ MORE: Malnutrition and weight loss
Podcast for people affected by cancer
Listen now
More resources
A/Prof Martin Batstone, Oral and Maxillofacial Surgeon and Director of the Maxillofacial Unit, Royal Brisbane and Women’s Hospital, QLD; Polly Baldwin, 13 11 20 Consultant, Cancer Council SA; Martin Boyle, Consumer; Dr Teresa Brown, Assistant Director Dietetics, Royal Brisbane and Women’s Hospital, Honorary Associate Professor, University of Queensland, QLD; Dr Hayley Dixon, Head, Clinical Support Dentistry Department, WSLHD Oral Health Services, Public Health Dentistry Specialist, NSW; Head and Neck Cancer Care Nursing Team, Royal Melbourne Hospital, VIC; Rhys Hughes, Senior Speech Pathologist, Peter MacCallum Cancer Centre, VIC; Dr Annette Lim, Medical Oncologist and Clinician Researcher – Head and Neck and Non-melanoma Skin Cancer, Peter MacCallum Cancer Centre, VIC; Dr Sweet Ping Ng, Radiation Oncologist, Austin Health, VIC; Deb Pickersgill, Senior Clinical Exercise Physiologist, Queensland Sports Medicine Centre, QLD; John Spurr, Consumer; Kate Woodhead, Physiotherapist, St Vincent’s Health, Melbourne, VIC; A/Prof Sue-Ching Yeoh, Oral Medicine Specialist, University of Sydney, Sydney Oral Medicine, Royal Prince Alfred Hospital, Chris O’Brien Lifehouse, NSW.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.