- Home
- Acute myeloid leukaemia (AML)
- What is AML?
What is AML?
Below we discuss how acute myeloid leukaemia (AML) starts, what causes it, who gets it, and more.
Learn more about:
For your community
Overview
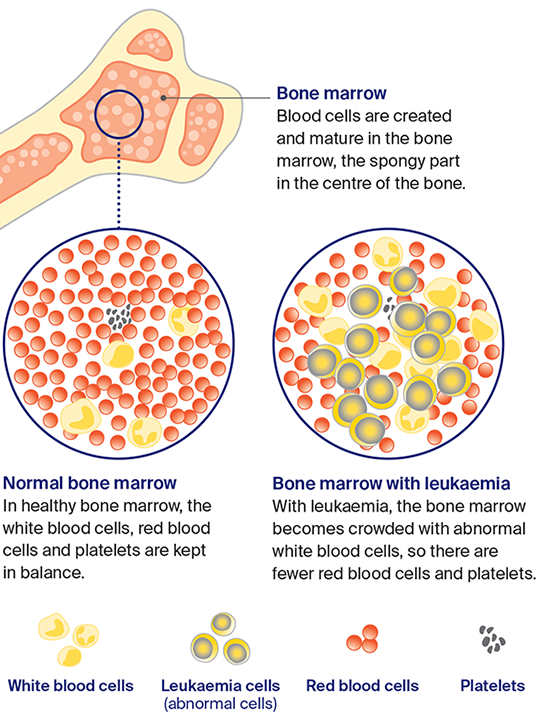
Acute leukaemia is a blood cancer that appears suddenly and grows quickly. It starts when undeveloped white blood cells – called blast cells – become cancerous. These abnormal blast cells are known as leukaemia cells. They multiply quickly and continue to divide but never mature into normal cells.
Because the leukaemia cells are undeveloped and abnormal, they don’t carry out the usual infection-fighting role of white blood cells. They also crowd out normal white blood cells, which then can’t work properly. This increases the risk of infections.
When the bone marrow fills with leukaemia cells, there is also little room for normal red blood cells and platelets. This can cause fatigue, bleeding problems and other health issues.
There are 2 main types of acute leukaemia: acute myeloid leukaemia (AML) and acute lymphoblastic leukaemia (ALL).
What is the difference between acute and chronic leukaemia?
While all types of leukaemia start in the bone marrow and affect how white blood cells are made, they are grouped according to the type of white blood cell affected, whether there are abnormalities in the bone marrow, and how quickly the disease develops.
Acute leukaemia usually affects undeveloped cells, occurs suddenly and grows quickly. Chronic leukaemia usually affects mature or partly developed cells, appears gradually and grows slowly over months to years.
For more on this see Chronic leukaemia (CLL) or Chronic leukaemia (CML).
What is the difference between AML and ALL?
The difference between AML and ALL is the type of white blood cell affected.
Acute myeloid leukaemia (AML) – Develops from myeloid cells. There are more than 20 subtypes of AML, including a subtype known as acute promyelocytic leukaemia (APML) that develops from immature myeloid cells called promyelocytes. APML is treated differently.
See more on AML risk factors and symptoms and read more on how AML is diagnosed and treated.
Acute lymphoblastic leukaemia (ALL) – Develops from lymphoid cells (lymphocytes). ALL can affect different types of lymphocytes, including B-cells or T-cells. B-cell ALL is the most common type, accounting for up to 80% of cases.
T-cell ALL is very similar to T-cell lymphoblastic lymphoma, and the 2 conditions are often treated the same way. In T-cell ALL, the abnormal lymphocytes are mainly in the blood and bone marrow, while in T-cell lymphoblastic lymphoma, the abnormal lymphocytes are in the lymph nodes.
See more on ALL risk factors and symptoms and read more on how ALL is diagnosed and treated.
Some people have a type of leukaemia called mixed-phenotype acute leukaemia (MPAL). This means the disease has features of both ALL and AML. MPAL may also be called biphenotypic acute leukaemia.
How leukaemia starts
The bone marrow produces 3 main types of blood cells: white cells, red cells and platelets. Leukaemia starts when abnormal white blood cells crowd the bone marrow and are pushed out into the bloodstream. Without treatment, they can spread to lymph nodes and some organs.
What causes AML?
The exact causes of acute leukaemia are not yet understood. Things known to increase the chance of developing the disease include:
- previous treatment with chemotherapy or radiation therapy
- having certain genetic disorders, such as Down syndrome
- exposure to high levels of radiation (e.g. nuclear accident)
- exposure to some chemicals, such as benzene
- smoking and/or obesity
- particular blood disorders, such as myelodysplasia (for AML)
- some viruses, such as Epstein-Barr virus, but this is rare.
Who gets AML?
About 5300 people are diagnosed with a form of leukaemia in Australia each year. About 1600 of these cases are acute leukaemia.
AML is the most common type of acute leukaemia in adults, with about 1200 people diagnosed each year. It becomes more common with age and mostly occurs after 60.
About 410 people are diagnosed with ALL each year. Of these, more than half are children and adolescents aged under 20, although ALL can occur at any age.
Children with acute leukaemia
This information is for adults diagnosed with acute leukaemia. As children and adults with acute leukaemia have similar tests, treatments and side effects, much of the information in this section will also apply to children. However, no 2 cases of acute leukaemia are the same, so it is important to discuss your child’s case in detail with their doctors. See more information about children with acute leukaemia.
The blood
Blood is pumped around your body to provide oxygen and nutrients to your tissues, and to remove waste products. It is made up of blood cells carried in a clear fluid called plasma.
All blood cells live for a limited time and need to be continually replaced. Most are made in the bone marrow, which is the spongy part in the centre of bones.
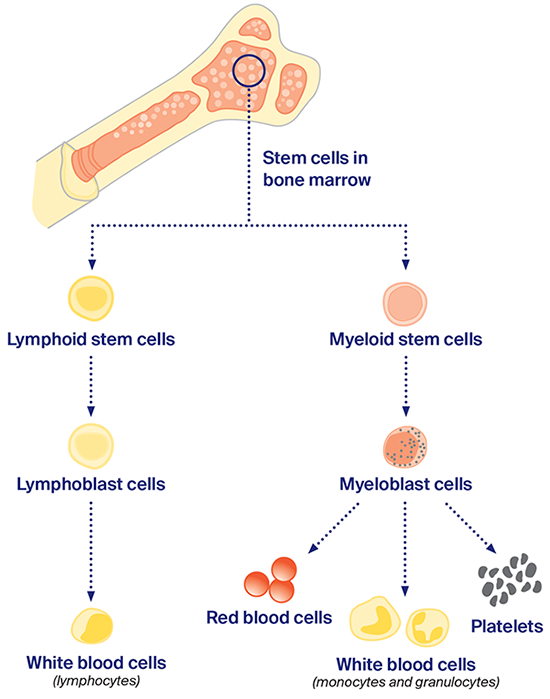
Bone marrow contains blood stem cells. These are unspecialised cells that usually grow into one of the 3 main types of blood cells: white blood cells, red blood cells or platelets. Each type of blood cell has a specific job to do.
 | White blood cells – fight infection. |
 | Red blood cells – carry oxygen around the body. |
 | Platelets – help the blood clot. |
There are 2 families of blood stem cells: lymphoid and myeloid. These develop into different types of white blood cells that can be affected by different types of leukaemia.
When myeloid stem cells grow abnormally, this is called acute myeloid leukaemia (AML); when lymphoid stem cells grow abnormally, this is called acute lymphoblastic leukaemia (ALL).
Blood stem cell families
Stem cells divide into 2 families (lymphoid or myeloid), then become immature cells (lymphoblast or myeloblast cells). If cells are normal, they develop into different kinds of mature cells.
What is the lymphatic system?
The lymphatic system is part of the immune system, which protects the body against disease and infection. It is a network of vessels, tissues and organs.
| Lymph vessels | These thin tubes are found throughout the body. They carry lymph fluid. |
| Lymph fluid | This clear fluid travels to and from the tissues in the body, carrying nutrients and taking away bacteria, viruses, abnormal cells and cell debris. |
| Lymph nodes | These are small bean-like structures in the neck, underarms, chest, abdomen and groin. Lymph nodes filter toxins, help fight infections, and produce some blood cells. They may also be called lymph glands. |
| Spleen | This is an organ in the abdomen. It clears out old or damaged blood cells. |
Sometimes leukaemia cells build up in the lymph nodes or spleen. When this happens, it can stop the lymphatic system from working properly and increase the risk of infections.
For an overview of what to expect during all stages of your cancer care for AML or ALL, visit www.cancer.org.au/cancercareguides. Here you will find short guides to what is recommended, from diagnosis to treatment and beyond.
What is blood cancer?
| What is cancer? | Cancer is a disease of the cells. Cells are the body’s basic building blocks – they make up blood, tissues and organs. The body is constantly making new cells to help us grow, replace worn-out tissue and heal injuries. |
| How do cells normally work? | Normally, cells multiply and die in an orderly way, so that each new cell replaces one lost. Sometimes, however, cells become abnormal and keep growing. These abnormal cells may turn into cancer. |
| Types of cancer | In solid cancers, such as breast cancer, the abnormal cells form a mass or lump called a tumour. In some cancers, such as leukaemia, the abnormal cells build up in the blood. |
| What happens in leukaemia? | In leukaemia, white blood cells grow abnormally and multiply in such a way that they crowd the bone marrow. This can reduce the bone marrow’s ability to produce normal levels of other blood cells, which affects the way the rest of the body works. The abnormal cells then move from the bone marrow into the bloodstream. |
| How does leukaemia progress? | As leukaemia progresses, the bone marrow produces more abnormal white blood cells and fewer normal blood cells. As the abnormal white blood cells build up, they can spread from the blood to the lymph nodes, spleen, liver, lungs and kidneys. Without treatment, leukaemia will increasingly affect the way the body works. |
| Advances in leukaemia treatment | Recent advances in treatment have seen the outlook for people with acute leukaemia improve. The disease can often be kept under control for years, and many people can live full lives after treatment finishes. |
More resources
Dr Jonathan Sillar, Haematologist, Calvary Mater Newcastle (clinical review); Dr Scott Dunkley, Haematologist, Royal Prince Alfred Hospital and Chris O’Brien Lifehouse; Sharon Frazer, Consumer; Dr Robin Gasiorowski, Staff Specialist, Haematology, Concord Hospital; Prof Angela Hong, Radiation Oncologist, Chris O’Brien Lifehouse, and Clinical Professor, The University of Sydney; Yvonne King, 13 11 20 Consultant, Cancer Council NSW; Heather Mackay, Clinical Nurse Consultant – Haematology, Westmead Hospital; Katelin Mayer, Clinical Nurse Consultant, Cancer Outreach Team, Nelune Comprehensive Cancer Centre.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.