- Home
- Bladder cancer
- Muscle-invasive bladder cancer treatment
- Surgery: cystectomy
Surgery: cystectomy
Some people with muscle-invasive disease have surgery to remove the bladder (cystectomy). This may also be recommended for high-risk superficial bladder cancer (also called non-muscle-invasive bladder cancer or NMIBC) that has not responded to BCG. The surgeon usually needs to remove the whole bladder and nearby lymph nodes. This is called a radical cystectomy.
Learn more about:
- How the surgery is done
- Surgery to remove the bladder
- What to expect after surgery
- Sexuality and fertility after cystectomy
How the surgery is done
Surgery to remove the bladder (called a cystectomy) and create a urinary diversion is a complicated operation.
Different surgical methods may be used to remove the bladder:
- Open surgery makes one long cut (incision) in the lower abdomen. A cut is usually made from below the bellybutton to the pubic area.
- Keyhole surgery, also known as minimally invasive or laparoscopic surgery, makes several smaller cuts in the abdomen. Instruments are inserted through the cuts, sometimes with help from a robotic system.
It is important to have this surgery in a specialised centre with a surgeon who does a lot of cystectomies. In general, having an experienced surgeon is more important than the type of surgery. Talk to your surgeon about the pros and cons of each surgical method, and check what you’ll have to pay. Unless you are treated as a public patient in a public hospital, you are likely to have lots of costs not covered by Medicare or your health fund.
Surgery to remove the bladder
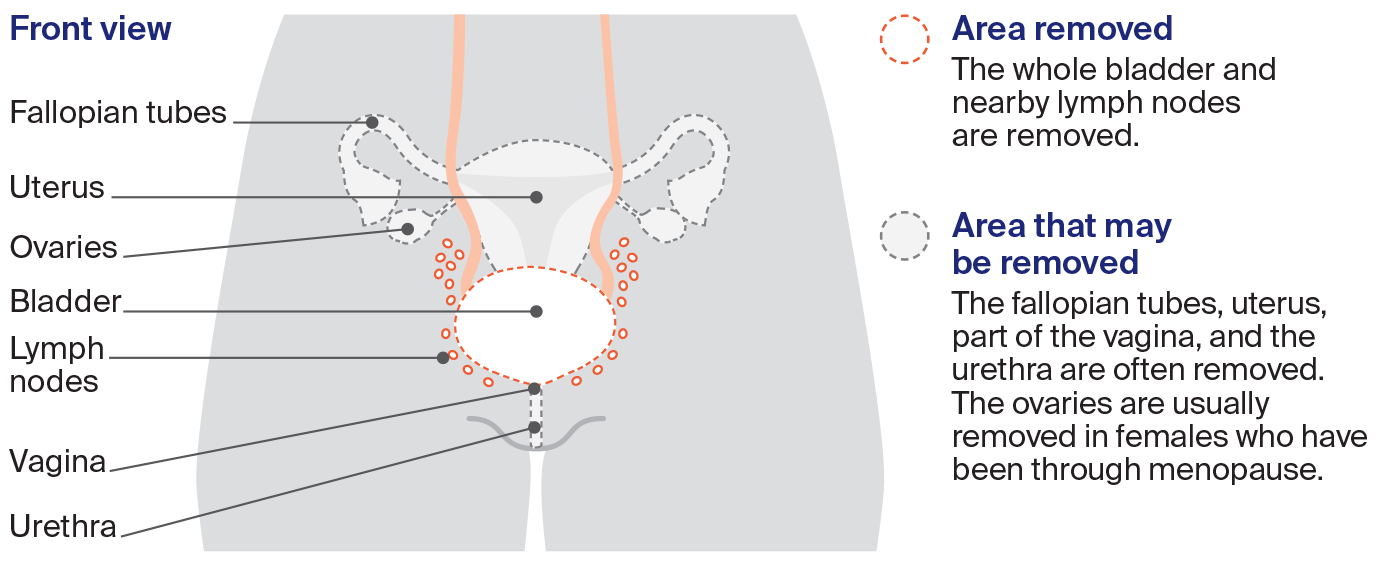
The most common operation for muscle-invasive bladder cancer is a radical cystectomy. The surgeon removes the whole bladder and nearby lymph nodes. Other organs may also be removed.
Cystectomy in males

Cystectomy in females
After a radical cystectomy, a urinary diversion is needed so your body can store and pass urine. For more information about urinary diversion.
What to expect after surgery
When you wake up after the operation, you will be in a recovery room near the operating theatre. Once you are fully conscious, you will be moved to intensive care or to the ward.
|
| Tubes and dripsYou may have an intravenous (IV) drip to give you fluid and medicine, and a tube in your abdomen to drain fluid from the operation area. These will be removed as you recover. |
Pain and discomfortAfter a major operation, it is common to feel some pain. You will be given pain medicine as a tablet (orally), through a drip (intravenously) or through a catheter inserted in the spaces in the spine (epidural) or along the wound (wound catheters). If you still have pain, let your doctor or nurse know and they may change your medicine. | |
Recovery timeYou will probably be in hospital for 1–2 weeks, but it can take 6–8 weeks to fully recover from a cystectomy. The recovery time will depend on the type of surgery, your fitness and whether you have any complications. | |
| | Passing urineBecause a radical cystectomy removes the whole bladder, the surgeon needs to create a new way for your body to store and pass urine. See more on urinary diversions. |
→ READ MORE: Sexuality and fertility after cystectomy
Podcast: Making Treatment Decisions
Listen now
More resources
Dr Prassannah Satasivam, Urologist and Robotic Surgeon, Epworth Hospitals and Cabrini Hospitals, VIC; Donna Clifford, Urology Nurse Practitioner, Royal Adelaide Hospital, SA; Marc Diocera, Genitourinary Nurse Consultant, Peter MacCallum Cancer Centre, VIC; Dr Renee Finnigan, Radiation Oncologist, Gold Coast University Hospital, QLD; Lisa Hann, 13 11 20 Consultant, Cancer Council SA; Dr Andrew Hirschhorn, Director of Allied Health and MQ Health Academy, MQ Health, Macquarie University, NSW; Anne Marie Lyons, Stomal Therapy Nurse, Concord Hospital and NSW Stoma Limited, NSW; John McDonald, Consumer; Prof Manish Patel, Urological Cancer and Robotic Surgeon, Westmead Hospital, Macquarie University Hospital, and The University of Sydney, NSW; Dr Jason Paterdis, Urological Surgeon, Brisbane Urology Clinic, QLD; Graeme Sissing, Consumer; Prof Martin Stockler, Medical Oncologist, The University of Sydney, Concord Cancer Centre, and Chris O’Brien Lifehouse RPA, NSW.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.

