- Home
- Brain tumours
- Treatment
- Radiation therapy
Radiation therapy for brain cancer
Also known as radiotherapy, radiation therapy uses a controlled dose of radiation to kill or damage tumour cells in the area being treated. The radiation is usually in the form of x-ray beams.
Learn more about:
- How radiation therapy is given
- How often will you have it?
- Stereotactic radiosurgery (SRS)
- Stereotactic radiation therapy (SRT)
- Proton therapy
- Wearing an immobilisation mask
- Side effects of radiation therapy
- Video: What is radiation therapy?
How radiation therapy is given
For gliomas, radiation therapy is usually given after surgery, and sometimes with chemotherapy (chemoradiation). Before you start radiation therapy, a radiation therapist will take measurements of your body and do a CT or MRI scan to work out the precise area to be treated.
Treatment is carefully planned to do as little harm as possible to the healthy brain tissue near the tumour. Radiation therapy itself is painless, though you may experience some side effects. Your treatment team will discuss these with you before you begin treatment.
If you are having radiation therapy for a brain tumour, you will wear a special plastic mask over your face. If you are having radiation therapy for a spinal cord tumour, some small marks may be tattooed on your skin to show the treatment area.
For more on this, see our general section on Radiation therapy.
For high-grade glioblastomas, radiation therapy is usually combined with chemotherapy. This is called chemoradiation. The chemotherapy drugs make the cancer cells more sensitive to radiation therapy.
How often will you have it?
How often you have radiation therapy (the treatment course) will depend on the size and type of tumour. Usually it is given once a day, from Monday to Friday, for several weeks (often 3 or 6 weeks, but this varies person to person).
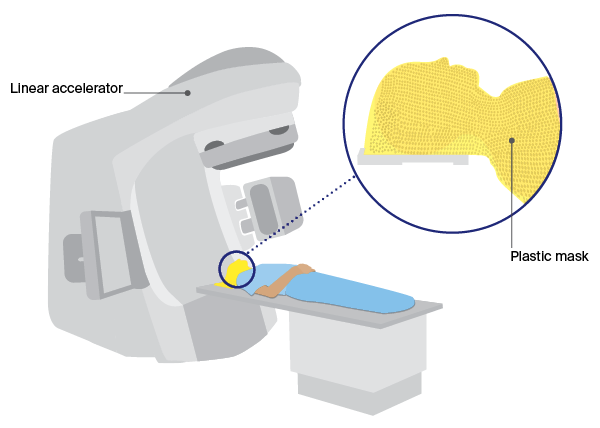
During treatment, you will lie on a table under a machine called a linear accelerator (LINAC). Most machines use daily imaging scans to check you are in the correct position for treatment.
Each treatment will last for about 10–15 minutes.
Stereotactic radiosurgery (SRS)
Stereotactic radiosurgery (SRS) is a specialised type of radiation therapy, not a type of surgery, and no cuts are made in the skull.
A specialised radiation machine is used to give very precisely targeted radiation to the tumour. Machine types include LINAC, Gamma Knife and CyberKnife. They deliver a high dose of radiation to the tumour while the surrounding healthy brain tissue receives very little.
SRS is not suitable for all types of brain tumours. It may be offered when neurosurgery is not possible, or as an alternative. It is mostly used for cancers that have spread to the brain from another part of the body. Some meningiomas, pituitary tumours, schwannomas, and occasionally gliomas that have come back, may be treated this way.
Often, only 2 or 3 doses of SRS are needed (though you may have 1–5 doses as treatment is personalised). A treatment session may last 15–45 minutes, depending on the type of radiosurgery given. You will need to wear a special mask or frame during the treatment. You will usually be able to go home after the session ends.
Stereotactic radiation therapy (SRT)
A stereotactic radiosurgery machine may also be used to deliver a longer course of radiation, particularly for benign brain tumours. This is called stereotactic radiation therapy or SRT. The treatment is given as multiple small daily doses.
If you feel anxious before your radiation therapy sessions, you may find it helpful to listen to the meditation and relaxation exercises in our Finding Calm During Cancer podcast. Or ask to speak to a social worker or psychologist for support.
Wearing an immobilisation mask
You’ll need to wear an immobilisation mask during radiation therapy to the brain. It helps keep your head still so that the radiation is targeted at the same area during each session. The mask is made to fit you and fixed to the table when the radiation treatment is given.
The mask is made of a tight-fitting plastic mesh that you can see and breathe through. It may feel strange and confined but you usually only wear it for about 10 or 20 minutes at a time. For some people, especially those with claustrophobia, the thought of wearing the mask can feel overwhelming.
The team may suggest that you try relaxation or breathing exercises or a psychologist can give you strategies to try. You may also be offered medicine to help you relax.
Tell the radiation therapist if wearing the mask makes you feel anxious. With support, many people get used to wearing it.
Proton therapy
This uses protons rather than x-ray beams. Protons are tiny parts of atoms with a positive charge. Proton therapy is used for some types of brain and spinal cord tumours, and tumours near sensitive areas.
A proton therapy machine has been installed in South Australia. It is hoped it will start treating patients soon. Currently, there is funding in special cases to allow Australians to travel overseas for proton therapy.
Side effects of radiation therapy
Radiation therapy side effects generally occur in the treatment area. They are usually temporary, but some may last for a few months or years, or be permanent. The side effects vary depending on whether the tumour is in the brain or spinal cord.
They may include:
| nausea | can occur several hours after treatment |
| headaches | can occur throughout the course of treatment |
| tiredness or fatigue | worse at the end of treatment; can continue to build after treatment, but usually improves over a month or so |
| dry, itchy, red, sore or flaky skin | may occur in the treatment area; is usually mild and happens at the end of the treatment course and lasts 1–2 weeks before going away |
| hair loss | may occur in a patch in the area of the head receiving treatment; usually temporary but in some cases permanent; if hair grows back, the texture or colour may be different |
| dulled hearing | may occur if fluid builds up in the middle ear and is usually temporary but may be permanent |
Radiation therapy side effects for spinal cord tumours may include sore or dry throat and swallowing problems (if the neck area is treated) or diarrhoea (if the lower spine is treated). Both are temporary. Talk to your radiation oncology team about how to manage any side effects.
A small number of adults who have had radiation therapy to the brain have side effects that appear months or years after treatment. These are called late effects, and can include symptoms such as poor memory, confusion and headaches.
High-dose radiation to the pituitary gland can cause it to produce too little of some hormones. This can affect body temperature, growth, sleep, weight and appetite. The hormone levels in your pituitary gland will be monitored during and after treatment.
→ READ MORE: Chemotherapy for brain cancer
Video: Radiation therapy for brain cancer
Watch this video to learn more about how radiation therapy is used to treat brain tumours.
Podcast: Making Treatment Decisions
Listen to more episodes from our podcast for people affected by cancer
More resources
Prof Lindy Jeffree, Director of Neurosurgery, Alfred Health, VIC; Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA; Prof Tamara Ownsworth, Clinical Neuropsychologist and Research Director, The Hopkins Centre, Griffith University, QLD; A/Prof Hao-Wen Sim, Medical Oncologist, The Kinghorn Cancer Centre and Chris O’Brien Lifehouse, NSW; Megan Trevethan, Clinical Specialist Occupational Therapy – Cancer and Lymphoedema Services, Princess Alexandra Hospital, QLD; Chris Twyford, Cancer Specialist Nurse, Canberra Health Services, Cancer and Ambulatory Support, ACT; Dr Adam Wells, Clinical Academic Consultant Neurosurgeon, The University of Adelaide, Royal Adelaide Hospital, SA.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.