- Home
- About Cancer
- Advanced cancer
- Facing end of life
- Physical changes
- Tiredness and fatigue
Tiredness and fatigue
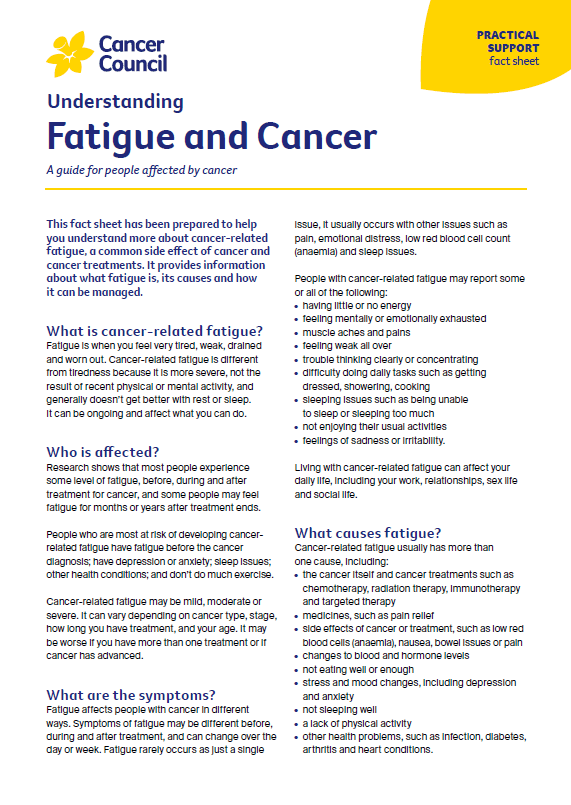
Most people with a terminal illness feel extreme or constant tiredness (fatigue). Try to pace yourself and save your energy for the activities that are most important to you. An occupational therapist may be able to help with equipment at home to reduce the energy needed for daily activities such as showering.
Fatigue may affect your ability to think clearly and make decisions. You will also probably be told when you need to stop driving and doing other activities. This can be frustrating, particularly if you are trying to put your affairs in order. You may want to deal with any demanding or practical concerns at a time of day when you have more energy.
While some people sleep a lot at the end of life, others find it hard to sleep, which can make fatigue worse. If you’re having trouble sleeping, it may be because of anxiety, pain, a side effect of a medicine you are taking or a change in your sleep-wake cycle. Let your health care or palliative care team know. They may be able to adjust your medicines or offer another medicine to help you sleep. They may suggest you try complementary therapies such as meditation and relaxation. Improving the quality of your sleep will improve the quality of your waking hours.
For more on this, see Fatigue and cancer.
→ READ MORE: Finding the right pain relief
The biggest side effect of the medication he started last year has been fatigue. He feels like he could sleep forever.
Susan
Podcast: Managing Cancer Fatigue
Listen to more of our podcast for people affected by cancer
More resources
Prof Jane Phillips, Head, School of Nursing and Professor, Centre for Healthcare Transformation, Queensland University of Technology and Emerita Professor Palliative Nursing, University of Technology Sydney, NSW; Prof Meera Agar, Palliative Care Physician, Professor of Palliative Medicine, University of Technology Sydney, IMPACCT, Sydney, NSW; Sandra Anderson, Consumer; A/Prof Megan Best, The University of Notre Dame Australia and The University of Sydney, NSW; Prof Lauren Breen, Psychologist and Discipline Lead, Psychology, Curtin University, WA; David Dawes, Manager, Spiritual Care Department, Peter MacCallum Cancer Centre, VIC; Rob Ferguson, Consumer; Gabrielle Gawne-Kelnar, Counsellor, Psychotherapist and Social Worker, One Life Counselling & Psychotherapy, NSW; Justine Hatton, Senior Social Worker, Southern Adelaide Palliative Services, Flinders Medical Centre, SA; Caitlin MacDonagh, Clinical Nurse Consultant, Palliative Care, Royal North Shore Hospital, Northern Sydney Local Health District, NSW; McCabe Centre for Law and Cancer; Palliative Care Australia; Belinda Reinhold, Acting Lead Palliative Care, Cancer Council QLD; Xanthe Sansome, National Program Director, Advance Care Planning Australia; Kirsty Trebilcock, 13 11 20 Consultant, Cancer Council SA.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.
Need to talk?
Support services
Caring for someone with cancer
Speak to a health professional or to someone who has been there, or find a support group or forum
Cancer Council Online Community
A community forum – a safe place to share stories, get tips and connect with people who understand
Cancer information
Relaxation and meditation
Learn how relaxation and meditation can help you both during and after cancer treatment, or listen to our relaxation and meditation audio tracks
Managing cancer side effects
Strategies for coping with some of the physical issues that can occur with cancer