Lymphoedema
Discover what lymphoedema is and how it can affect movement and activity. Learn more about its causes, symptoms, and treatment options.
Learn more about
- Overview
- Symptoms of lymphoedema
- How to find a lymphoedema professional
- How to prevent or manage lymphoedema
Overview
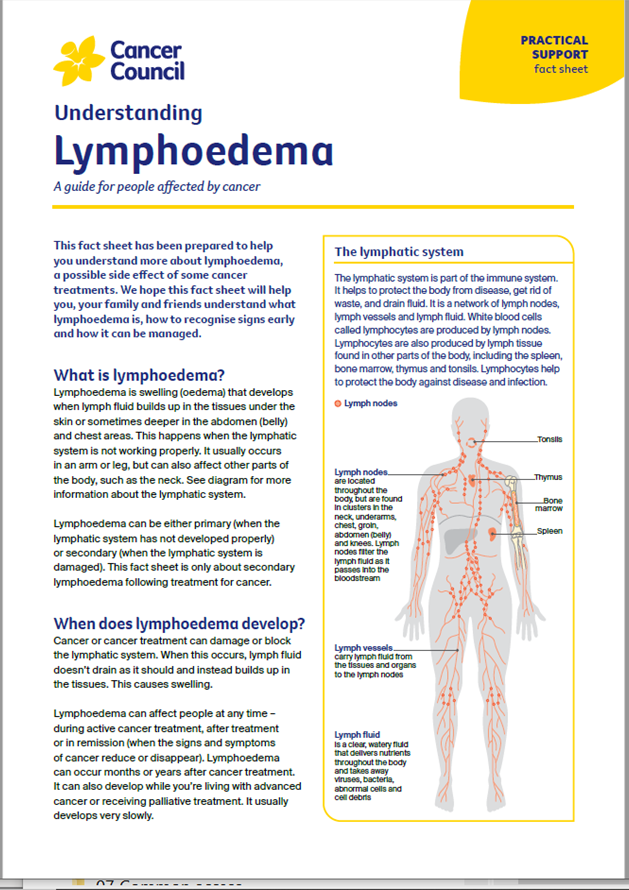
When lymph fluid builds up in the tissues under the skin, it can cause swelling (oedema). This is known as lymphoedema. It can happen if lymph nodes have been removed during surgery or damaged by infection, injury or radiation therapy. Lymphoedema may appear during treatment or months or years later.
Lymphoedema can occur after treatment for many different cancers, but is more common in people treated for gynaecological (vulvar, vaginal, ovarian, uterine and cervical), breast and prostate cancers or melanoma. Whether or not you develop lymphoedema after treatment depends on the location of the cancer, its stage and the type of treatment you had. Not everyone who is at risk will develop it.
Symptoms of lymphoedema
Having lymphoedema can make movement and some types of activity difficult. Swelling usually happens in an arm or leg, but it can also affect other areas of the body.
The main signs of lymphoedema include:
- visible swelling
- aching, tingling or feelings of tightness or heaviness
- not being able to fully move the affected limb
- clothing, shoes or jewellery feeling tighter than usual
- pitting of the skin (when gentle pressure leaves a small dent).
How to find a lymphoedema professional
To find a health professional who specialises in the management of lymphoedema, visit the Australasian Lymphology Association and click on “Find a Practitioner”. This may be an occupational therapist, physiotherapist or nurse with special training.
How to prevent or manage lymphoedema
- Treat lymphoedema early so you can deal with the problem quickly and avoid symptoms becoming worse.
- If you are at risk of developing lymphoedema, see a lymphoedema practitioner for regular check-ups rather than waiting for signs to appear. They may monitor the amount of fluid in your body using a painless electric charge (bioimpedance spectroscopy).
- Keep physically active to help the lymph fluid flow. Do regular exercise such as swimming, cycling or using light weights.
- Keep the skin healthy and unbroken to reduce the risk of infection. Avoid cuts, scratches, bites and injections in the affected area. If you shave, use an electric razor to minimise cutting the skin.
- Moisturise your skin daily to prevent dry, irritated skin. If you have lymphoedema, ask your lymphoedema practitioner about suitable creams and lotions.
- Protect your skin from the sun.
- Maintain a healthy body weight. Being overweight can be a risk factor for developing lymphoedema.
- Avoid wearing jewellery or clothing that puts pressure on the affected area or leaves marks on your skin.
- Take care cutting your toenails or see a podiatrist to look after your feet.
- Wear a professionally fitted compression garment, if advised by your lymphoedema practitioner.
- Seek medical help urgently if you think you have an infection in the affected area.
Learn more about lymphoedema.
Although I’d had lots of lymphoedema education, I actually missed the signs and didn’t realise I had it until I developed a skin infection called cellulitis.
Suzanne
→ READ MORE: Changes in thinking and memory
More resources
Prof Michael Jefford, Medical Oncologist and Director, Australian Cancer Survivorship Centre, Peter MacCallum Cancer Centre, VIC (clinical review); Lucy Bailey, Nurse Counsellor, Cancer Council Queensland; Philip Bullas, Consumer; Dr Kate Gunn, Clinical Psychologist and Senior Research Fellow, Department of Rural Health, University of South Australia, SA; Rosemerry Hodgkin, 13 11 20 Consultant, Cancer Council WA; Prof David Joske, Clinical Haematologist, Sir Charles Gairdner Hospital and Clinical Professor of Medicine, The University of Western Australia, WA; Kim Kerin-Ayres, Clinical Nurse Consultant, Cancer Survivorship, Concord Hospital, NSW; Sally Littlewood, Physiotherapist, Seymour Health, VIC; Georgina Lohse, Social Worker, GV Health, VIC; Melanie Moore, Exercise Physiologist and Clinical Supervisor, University of Canberra Cancer Wellness Clinic, ACT; June Savva, Senior Clinician Dietitian, Nutrition and Dietetics, Monash Cancer Centre, Monash Health, VIC; Dr Elysia Thornton-Benko, Specialist General Practitioner and Research Fellow, University of New South Wales, NSW; Prof Janette Vardy, Medical Oncologist, Concord Cancer Centre and Professor of Cancer Medicine, The University of Sydney, NSW; Lyndell Wills, Consumer.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.