- Home
- About Cancer
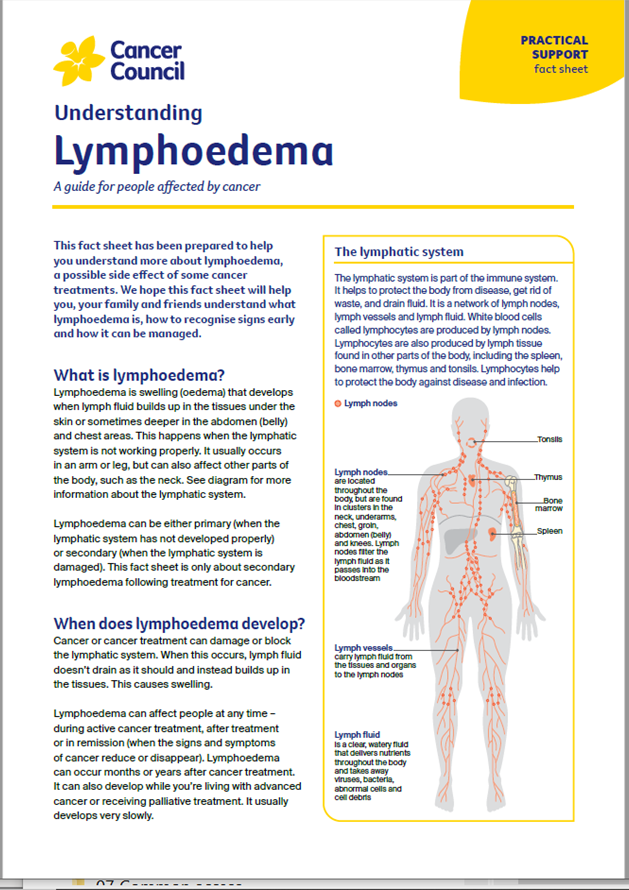
- Managing side effects
- Lymphoedema
- Early signs
Early signs of lymphoedema
Finding lymphoedema before you notice any signs can reduce the risk of developing swelling.
Learn more about:
What is early intervention?
If you are at risk of lymphoedema, ask your treatment team if regular screening check-ups are recommended for you and available near where you live. Early detection and early intervention using education, compression garments and exercise helps to reduce the impact of lymphoedema.
What are the early warning signs?
Taking action quickly can reverse mild lymphoedema and help reduce the risk of developing severe lymphoedema. As soon as you notice any warning signs in the affected area, it’s important to see your lymphoedema practitioner or doctor.
Early warning signs include:
- feeling of tightness, heaviness or fullness
- aching in the affected area
- swelling that comes and goes or is more noticeable at the end of the day (or on waking for head and neck cancer)
- tighter clothing, shoes or jewellery
- not being able to fully move the affected limb
- pitting of the skin (when gentle pressure leaves an indent on the skin).
Contact a lymphoedema practitioner if you notice any of these signs or are unsure about your risk of developing lymphoedema.
What happens if lymphoedema is left untreated?
If left untreated, lymphoedema can progress and cause a range of problems, including:
- trouble moving around and doing usual activities
- discomfort and sometimes pain
- difficulty fitting into clothes or shoes
- an increased risk of infections
- further hardening of the skin
- lymph fluid leaking from the skin (lymphorrhoea)
- very rarely, the development of angiosarcoma, a type of soft tissue cancer.
My experience is that lymphoedema is very manageable if you notice the signs early.
Susanne
→ READ MORE: Reducing your risk of lymphoedema
Podcast: Coping with a cancer diagnosis
Listen to more of our podcast for people affected by cancer
More resources
A/Prof Louise Koelmeyer, Director, Australian Lymphoedema Education, Research and Treatment (ALERT) Program, and Associate Professor, Macquarie University, NSW; Prof John Boyages AM, Founding Director and Honorary Professor at the ALERT Program, Macquarie University, NSW; Dr Nicola Fearn, Occupational Therapist and Accredited Lymphoedema Therapist, The Lymphoedema Clinic Wollongong, and Senior Research Officer, St Vincent’s Hospital Sydney, NSW; Jennifer Gilbert, Clinical Nurse Consultant – Lymphoedema, Icon Cancer Centre, Chermside, QLD; Megan Howard, Senior Physiotherapist and Lymphoedema Physiotherapist, Peter MacCallum Cancer Centre, VIC; Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA; Dr Amanda Pigott, Clinical Specialist Occupational Therapy, Princess Alexandra Hospital, QLD; Prof Neil Piller, Director, Lymphoedema Clinical Research Unit, College of Medicine and Public Health, Flinders University, SA, and Patron, Lymphoedema Association of Australia; Ashlynne Pointon, Consumer; Dr Cathie Poliness, Breast Surgeon, Peter MacCallum Cancer Centre, VIC; Tara Redemski, Senior Physiotherapist – Cancer and Blood Disorders, Gold Coast University Hospital, QLD.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.