- Home
- Liver cancer
- Treatment
- Drug therapies
Drug therapies for liver cancer
Two types of drug therapies are available to treat primary liver cancer: immunotherapy and targeted therapy.
Drug therapies (sometimes called systemic therapies) can spread throughout the whole body to treat cancer cells wherever they may be, which can be helpful for cancer that has spread (metastatic cancer).
Learn more about:
- Immunotherapy
- Immunotherapy side effects
- Targeted therapy
- Targeted therapy side effects
- Video: What are drug therapies?
Immunotherapy
This is a type of drug treatment that helps the body’s own immune system to fight cancer cells. Immunotherapy drugs known as checkpoint inhibitors block proteins that stop immune cells from recognising and destroying the cancer cells. Once the proteins are blocked, the immune cells can recognise and attack the cancer.
A checkpoint inhibitor called atezolizumab is an immunotherapy drug subsidised on the Pharmaceutical Benefits Scheme (PBS) to treat some types of primary liver cancer.
Atezolizumab, which is given in combination with a targeted therapy drug called bevacizumab, is often the first drug treatment used for primary liver cancer.
Immunotherapy drugs are delivered by drip into a vein (intravenously), which may take 1–3 hours. Treatments are usually given every three weeks and your doctor will discuss with you how often and how many treatments will be needed.
It helps to focus on what is happening now, what is actually known – not all the possibilities. One step at a time.
Sam
What are the possible side effects?
Immunotherapy can have different side effects for different people. These mostly happen when the immune system becomes overstimulated and attacks organs such as the skin, bowel, liver or hormone-producing glands.
These immune-related side effects can happen when you are having treatment or in the weeks, months, or even years, afterwards. In rare cases, side effects can be the sign of serious complications, so even mild side effects should be reported to your doctor.
Immune-related side effects may need to be treated with drugs to help control the immune response (called immunosuppressive drugs), and the immunotherapy may need to be stopped.
If you are unable to manage the side effects of immunotherapy, your doctor may recommend switching to targeted therapy.
When you start immunotherapy, you may be given an alert card so you can let all health professionals know that you are having this treatment. This ensures that you are given the best treatment if you develop side effects.
For more on this, see our general section on Immunotherapy.
Targeted therapy
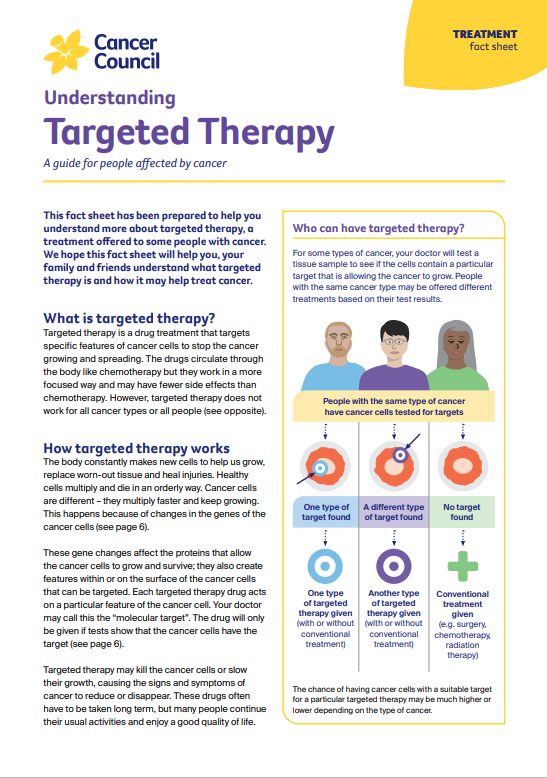
This type of treatment targets specific features of cancer cells to stop the cancer growing and spreading. People who have advanced liver cancer and are unable to take immunotherapy may be offered targeted therapy drugs such as sorafenib or lenvatinib. These drugs are both subsidised by the PBS for some types of primary liver cancer. They are given as tablets that you swallow. Your doctor will explain when to take them.
What are the possible side effects?
The side effects of sorafenib and lenvatinib may include skin rash, diarrhoea, fatigue and high blood pressure. These side effects can usually be managed without having to completely stop treatment.
Your treatment team will monitor you while you are taking targeted therapy drugs. If you find the side effects of targeted therapy difficult to manage, your doctor may recommend switching to another drug.
Generally, targeted therapy is continued for as long as there is benefit. If liver cancer progresses despite treatment with sorafenib or lenvatinib, your doctor may talk to you about trying another targeted therapy drug.
For more on this, see our general section on Targeted therapy.
Drug treatment for advanced liver cancer is changing quickly and new treatments may become available in the near future. You may also be able to get new drugs through clinical trials. Talk to your doctor about the latest developments and whether there are any suitable clinical trials for you.
→ READ MORE: Palliative treatment
Video: What are drug therapies?
Watch this short video to learn more about targeted and immunotherapy
Podcast: Making Treatment Decisions
Listen to more episodes from our podcast for people affected by cancer
More resources
A/Prof Simone Strasser, Hepatologist, AW Morrow Gastroenterology and Liver Centre, Royal Prince Alfred Hospital and The University of Sydney, NSW (clinical update); A/Prof Siddhartha Baxi, Radiation Oncologist and Medical Director, GenesisCare, Gold Coast, QLD (clinical update); Prof Katherine Clark, Clinical Director of Palliative Care, NSLHD Supportive and Palliative Care Network, Northern Sydney Cancer Centre, Royal North Shore Hospital, NSW; Anne Dowling, Hepatoma Clinical Nurse Consultant and Liver Transplant Coordinator, Austin Health, VIC; A/Prof Koroush Haghighi, Liver, Pancreas and Upper Gastrointestinal Surgeon, Prince of Wales and St Vincent’s Hospitals, NSW; Karen Hall, 131120 Consultant, Cancer Council SA; Dr Brett Knowles, Hepato-Pancreato-Biliary and General Surgeon, Royal Melbourne Hospital, Peter MacCallum Cancer Centre and St Vincent’s Hospital, VIC; Lina Sharma, Consumer; David Thomas, Consumer; Clinical A/Prof Michael Wallace, Department of Hepatology and Western Australian Liver Transplant Service, Sir Charles Gairdner Hospital Medical School, The University of Western Australia, WA; Prof Desmond Yip, Clinical Director, Department of Medical Oncology, The Canberra Hospital, ACT.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.