- Home
- Lung cancer
- Treatment
- Radiation therapy
Radiation therapy for lung cancer
Also known as radiotherapy, radiation therapy uses radiation to target and kill cancer cells. This reduces the risk of the cancer growing or spreading. It uses advanced technology to focus the radiation on the cancer and avoid the normal parts of the body.
Learn more about:
- Overview
- Standard external beam radiation therapy (EBRT)
- Stereotactic body radiation therapy (SBRT)
- Planning radiation therapy
- Having radiation therapy
- Side effects of radiation therapy
- Video: What is radiation therapy?
- Podcast: Making Treatment Decisions
Overview
You may be given radiation therapy on its own, or after surgery or chemotherapy, or at the same time as chemotherapy (called chemoradiation). When you have it depends on the stage of the cancer.
Radiation therapy may be recommended to treat the primary tumour in the lung:
- if you are unable to have surgery for stage 1 lung cancer
- if you chose not to have surgery
- where a surgery is not able to be safely done to treat locally advanced (stage 3) NSCLC, or to treat limited-disease SCLC
- after surgery, if there is a risk of microscopic cancer cells left behind.
You may be offered radiation therapy as palliative treatment, to control the primary tumour in the lung or areas where the tumour has spread to, with the aim of relieving pain, breathlessness or other symptoms.
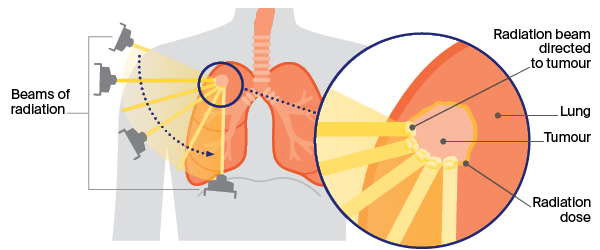
For lung cancer, radiation is usually delivered in the form of x-ray beams from a machine outside the body called a linear accelerator. This is known as external beam radiation therapy (EBRT) and can be done as standard EBRT or stereotactic radiation therapy (SBRT).
Standard external beam radiation therapy (EBRT)
This is usually given once a day, Monday to Friday; each daily treatment lasts for a few minutes. How many treatments you need will depend on the aim of the treatment. To control symptoms, it’s usually 1–2 weeks. Longer-term control is usually for 3–6 weeks.
Stereotactic body radiation therapy (SBRT)
Also called stereotactic body radiation therapy (SBRT) or stereotactic ablative body radiation (SABR), this can be given as a single dose or a number of doses. It targets a localised tumour with a very high dose of radiation. SBRT cannot be used safely if tumours are close to other organs, such as the windpipe.
How SBRT is done
External beam radiation uses a machine that gives high-dose radiation beams from different angles to precisely target the tumour.
Planning radiation therapy
Before treatment starts, you will have a planning session at the radiation therapy centre to work out the dose and position of the beams. During this session, you will have a CT scan to determine the area to be treated, and small marks will be put on your skin so the radiation therapists ensure your body is in the same position for every treatment.
You may have a 4-dimensional CT scan to record any movement of the cancer as you breathe. You may also be shown some breathing exercises to help your breathing stay as regular as possible.
Having radiation therapy
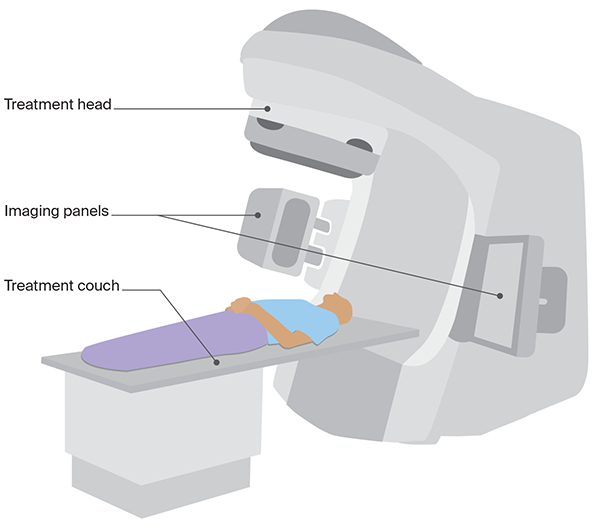
Each treatment day, a radiation therapist will help you lie in the position decided at the planning session. You will have an x-ray to check that the correct area is being treated.
When the treatment is being delivered, you will be alone in the room, but the radiation therapists will be able to hear you and talk to you from the monitoring area as there are speakers and a microphone in the room.
The radiation treatment itself takes only a few minutes, but a session may last about 20 minutes, depending on how complex the set-up process is.
Linear accelerator
Side effects of radiation therapy
Radiation therapy itself is painless, but it can affect some tissues and organs of the body. You may experience some side effects during or after radiation therapy, depending on the dose, the number of treatments and the part of the chest treated. Most side effects are temporary and improve a few weeks after treatment.
| Fatigue | Feeling tired is common after radiation therapy. You may need more rest or sleep, but gentle exercise and being physically active, if you are able to, is encouraged. Learn tips on managing fatigue. |
| Discomfort when swallowing and heartburn | If the cancer is in the centre of the chest and near the oesophagus, you may find swallowing uncomfortable, and develop heartburn. You may need to eat softer food and avoid hot drinks until you feel better. You may also be prescribed medicine by your radiation oncologist to control the pain until these side effects resolve. |
| Skin changes | Skin may become red and inflamed if the tumour is very close to the skin, but this is rare. Applying a moisturising cream and sun protection daily can help protect your skin. |
| Shortness of breath and cough | Radiation therapy may cause inflammation of the lungs. Called radiation pneumonitis, this may cause shortness of breath and/or a cough. This may happen during treatment, but it is more likely to appear 1–6 months after treatment ends. Radiation pneumonitis is usually temporary and can be treated. Side effects can change from one treatment session to the next and may build up over time. Tell the radiation oncology team about any side effects you have, as most can be managed. |
| Lung inflammation (pneumonitis) | Radiation therapy may cause inflammation of the lungs, called radiation pneumonitis. This may happen 2–12 months after the radiation has finished and usually doesn’t need any treatment. Occasionally, it can cause shortness of breath and/or a cough which may require treatment with steroids. Tell your radiation oncology team about any side effects you are concerned about, as most can be managed. |
Learn more about radiation therapy.
→ READ MORE: Chemotherapy for lung cancer
Video: What is radiation therapy?
Watch this short video to learn more about radiation therapy.
Podcast: Making Treatment Decisions
Listen to more of our podcast for people affected by cancer
Dr Malinda Itchins, Thoracic Medical Oncologist, Royal North Shore Hospital and Chris O’Brien Lifehouse, NSW; Dr Cynleen Kai, Radiation Oncologist, GenesisCare, VIC; Dr Naveed Alam, Thoracic Surgeon, St Vincent’s Hospital, Epworth Richmond, and Monash Medical Centre, VIC; Helen Benny, Consumer; Dr Rachael Dodd, Senior Research Fellow, The Daffodil Centre, NSW; Kim Greco, Specialist Lung Cancer Nurse Consultant, Flinders Medical Centre, SA; Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA; Marco Salvador, Consumer; Janene Shelton, Lung Foundation Australia – Specialist Lung Cancer Nurse, Darling Downs Health, QLD; Prof Emily Stone, Respiratory Physician, Department of Thoracic Medicine and Lung Transplantation, St Vincent’s Hospital Sydney, NSW; A/Prof Marianne Weber, Stream Lead, Lung Cancer Policy and Evaluation, The Daffodil Centre, NSW.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.