- Home
- Melanoma
- Treatment for advanced melanoma
- Targeted therapy
Targeted therapy for advanced melanoma
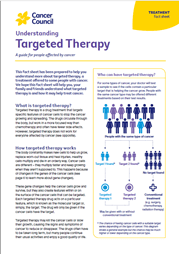
New types of drugs known as targeted therapy attack specific features of cancer cells to stop the cancer growing and spreading. Your doctor will check if the melanoma has a specific mutation before offering you a targeted therapy drug.
Learn more about:
- Having targeted therapy
- Side effects of targeted therapy
- Video: What is targeted therapy?
- Podcast: Immunotherapy & Targeted Therapy
Having targeted therapy
If a person has a BRAF mutation, they will get both a BRAF inhibitor and a MEK inhibitor. Three commonly used combinations include dabrafenib and trametinib; vemurafenib and cobimetinib; and encorafenib and binimetinib. Drugs for NRAS and C-KIT mutations may be available through clinical trials – talk to your doctor about whether one of these trials is right for you.
Targeted therapy drugs are generally taken as tablets (orally) once or twice a day, often for many months or even years. Cancer cells can become resistant to targeted therapy drugs over time. If this happens, your doctor may suggest trying another targeted therapy drug or another type of treatment.
Side effects of targeted therapy
The side effects of targeted therapy will vary depending on which drugs you are given. Common side effects include fever, tiredness, joint pain, rash and other skin problems, loss of appetite, nausea and diarrhoea.
Ask your treatment team how you can deal with any side effects.
For more on this, see our general section on Targeted therapy.
→ READ MORE: Radiation therapy for advanced melanoma
Video: What is targeted therapy?
Watch this short video to learn more about targeted and immunotherapy.
Podcast: Immunotherapy & Targeted Therapy
Listen to more episodes from our podcast for people affected by cancer
More resources
Prof H Peter Soyer, Chair in Dermatology and Director, Dermatology Research Centre, The University of Queensland, Diamantina Institute, and Consultant, Dermatology Department, Princess Alexandra Hospital, QLD; A/Prof Matteo Carlino, Medical Oncologist, Blacktown and Westmead Hospitals, Melanoma Institute Australia and The University of Sydney, NSW; Prof Anne Cust, Deputy Director, The Daffodil Centre, The University of Sydney and Cancer Council NSW, Chair, National Skin Cancer Committee, Cancer Council and faculty member, Melanoma Institute Australia; Prof Diona Damian, Dermatologist, Head of Department, Dermatology, The University of Sydney at Royal Prince Alfred Hospital, NSW, and Melanoma Institute Australia; A/Prof Paul Fishburn, General Practitioner – Skin Cancer, Norwest Skin Cancer Clinic, NSW and The University of Queensland; Claire Kelly, National Support Manager, and Emma Zurawel, Telehealth Nurse, Melanoma Patients Australia; Prof John Kelly, Consultant Dermatologist, Victorian Melanoma Service, The Alfred Melbourne and Monash University, VIC; Liz King, Manager, Skin Cancer Prevention Unit, Cancer Council NSW; Lee-Ann Lovegrove, Consumer; Lynda McKinley, 13 11 20 Consultant, Cancer Council Queensland; Angelica Miller, Melanoma Community Support Nurse, Melanoma Institute Australia incorporating melanomaWA, and Cancer Wellness Centre, WA; Dr Amelia Smit, Research Fellow, Melanoma and Skin Cancer, The Daffodil Centre, The University of Sydney and Cancer Council NSW; Prof Andrew Spillane, Professor of Surgical Oncology, The University of Sydney, The Mater and Royal North Shore Hospitals, NSW, and Melanoma Institute Australia; Kylie Tilley, Consumer; A/Prof Tim Wang, Radiation Oncologist, Crown Princess Mary Cancer Centre, Westmead Hospital, NSW. We also thank the health professionals, consumers and editorial teams who have worked on previous editions of this title.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.