- Home
- Melanoma
- Treatment for early melanoma
- Removing lymph nodes
Removing lymph nodes
Many people with melanoma will not need to have any lymph nodes removed.
Learn more about:
Overview
Lymph nodes may need to be removed for several reasons:
Sentinel lymph node
If the melanoma is thicker than 1 mm or has high-risk features, you may have a sentinel lymph node biopsy at the same time as the wide local excision.
Further scans and treatment
If a sentinel node biopsy shows melanoma is found in the removed node, you will need to have regular imaging scans to check that the melanoma has not come back or spread. You may also be offered drug therapy to reduce the risk of the melanoma returning.
Lymph node dissection
If your lymph nodes feel or look swollen, and a fine needle biopsy confirms that a lymph node contains melanoma – you may need to have all the lymph nodes in that area removed under a general anaesthetic. This operation is called a lymph node dissection or lymphadenectomy, and may mean a longer stay in hospital. Your doctor may also suggest you have targeted therapy or immunotherapy before surgery (neoadjuvant treatment).
This treatment is best done at a melanoma unit.
Side effects of lymph node removal
Having your lymph nodes removed can cause side effects. These are likely to be milder if you only have a sentinel node biopsy.
Wound pain
Most people will have some pain after the operation, which usually improves as the wound heals. For some people, the pain may be ongoing, especially if lymph nodes were removed from the neck. Talk to your medical team about how to manage any pain.
Neck/shoulder/hip stiffness and pain
These are the most common problems if lymph nodes in your neck, armpit or groin were removed. You may find that you cannot move the affected area as freely as you could before the surgery. It may help to do gentle exercises or ask your GP or cancer care team to refer you to a physiotherapist.
Seroma/lymphocele
This is a collection of fluid in the area where the lymph nodes have been removed. It is a common side effect and appears straight after surgery. It usually gets better after a few weeks, but sometimes your surgeon may drain the fluid with a needle.
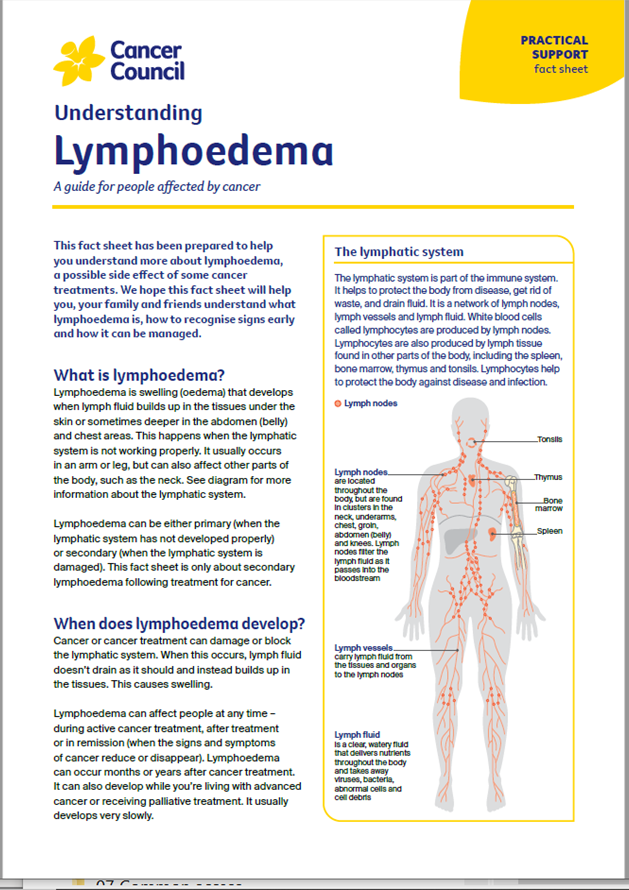
Lymphoedema
This is a swelling of the neck, arm or leg that may appear after the lymph nodes are removed. Lymphoedema happens when lymph fluid builds up in the affected part of the body because the treatment has impacted the lymphatic system.
Managing lymphoedema
Your risk of developing lymphoedema depends on the extent of the surgery and whether you’ve had radiation therapy.
Lymphoedema can develop a few weeks, or even several years, after treatment. Although this condition may be permanent, it can usually be managed, especially if treated at the earliest sign of swelling or heaviness.
A lymphoedema practitioner can help you manage lymphoedema. To find a trained practitioner, visit Australasian Lymphology Association or ask your doctor for a referral. You may need to wear a professionally fitted compression garment. Massage and regular exercise, such as swimming, cycling or yoga, can help the lymph fluid flow. Keeping the skin healthy can help reduce the risk of infection.
For more on this, see our general section on Lymphoedema.
Podcast: Making Treatment Decisions
Listen to more of our podcast for people affected by cancer
→ READ MORE: Further treatments for melanoma
More resources
Prof H Peter Soyer, Chair in Dermatology and Director, Dermatology Research Centre, The University of Queensland, Diamantina Institute, and Consultant, Dermatology Department, Princess Alexandra Hospital, QLD; A/Prof Matteo Carlino, Medical Oncologist, Blacktown and Westmead Hospitals, Melanoma Institute Australia and The University of Sydney, NSW; Prof Anne Cust, Deputy Director, The Daffodil Centre, The University of Sydney and Cancer Council NSW, Chair, National Skin Cancer Committee, Cancer Council and faculty member, Melanoma Institute Australia; Prof Diona Damian, Dermatologist, Head of Department, Dermatology, The University of Sydney at Royal Prince Alfred Hospital, NSW, and Melanoma Institute Australia; A/Prof Paul Fishburn, General Practitioner – Skin Cancer, Norwest Skin Cancer Clinic, NSW and The University of Queensland; Claire Kelly, National Support Manager, and Emma Zurawel, Telehealth Nurse, Melanoma Patients Australia; Prof John Kelly, Consultant Dermatologist, Victorian Melanoma Service, The Alfred Melbourne and Monash University, VIC; Liz King, Manager, Skin Cancer Prevention Unit, Cancer Council NSW; Lee-Ann Lovegrove, Consumer; Lynda McKinley, 13 11 20 Consultant, Cancer Council Queensland; Angelica Miller, Melanoma Community Support Nurse, Melanoma Institute Australia incorporating melanomaWA, and Cancer Wellness Centre, WA; Dr Amelia Smit, Research Fellow, Melanoma and Skin Cancer, The Daffodil Centre, The University of Sydney and Cancer Council NSW; Prof Andrew Spillane, Professor of Surgical Oncology, The University of Sydney, The Mater and Royal North Shore Hospitals, NSW, and Melanoma Institute Australia; Kylie Tilley, Consumer; A/Prof Tim Wang, Radiation Oncologist, Crown Princess Mary Cancer Centre, Westmead Hospital, NSW. We also thank the health professionals, consumers and editorial teams who have worked on previous editions of this title.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.