- Home
- Non-Hodgkin lymphoma
- Treatment
- Targeted therapy
Targeted therapy for non-Hodgkin lymphoma
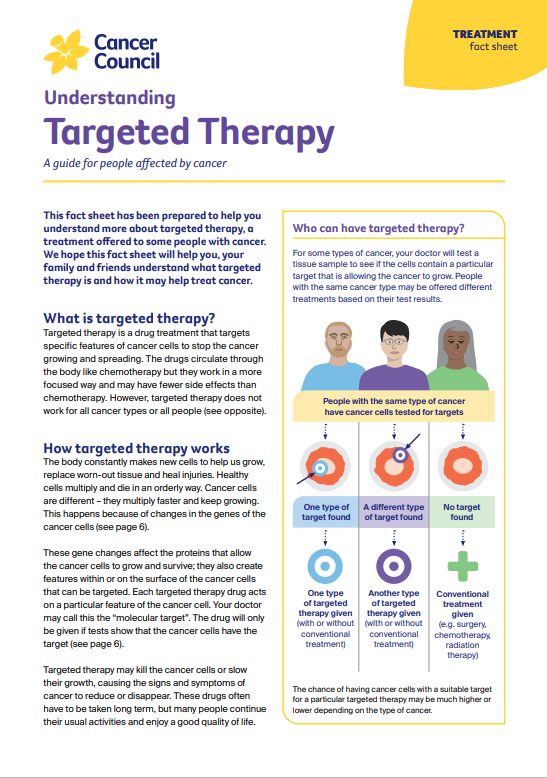
Targeted therapy drugs attack specific features of cancer cells to stop the cancer growing or to reduce its size.
Learn more about:
- What are monoclonal antibodies?
- Having monoclonal antibodies
- Side effects of targeted therapy
- Small molecule inhibitors
- Video: What is targeted therapy?
- Podcast: Immunotherapy & Targeted Therapy
What are monoclonal antibodies?
Some types of non-Hodgkin lymphoma are treated with a group of targeted therapy drugs called monoclonal antibodies.
The body’s immune system makes proteins called antibodies to help fight infections. Monoclonal antibodies are manufactured versions of these natural antibodies. They lock onto a protein on the surface of cells or surrounding tissues to affect how cancer cells grow and survive.
Because they work with the immune system, monoclonal antibodies may also be considered a form of immunotherapy.
There are different drugs available and your haematologist will discuss which combination of drugs is best for your situation.
| For CD20 proteins | Rituximab and obinutuzumab are used when the protein CD20 is found on B-cell non-Hodgkin lymphomas. Newer drugs for CD20 are becoming available in Australia. These work in the same way and are known as biosimilar drugs. These drugs do not work for T-cell or NK-cell lymphomas. |
| For CD30 proteins | Brentuximab vedotin is used when the protein CD30 is found in some B-cell and T-cell lymphomas. |
| Other drugs | Other targeted therapy drugs may be available through clinical trials. Ask your doctor about the latest developments in targeted therapy for non-Hodgkin lymphoma. |
Having monoclonal antibodies
Monoclonal antibodies are generally given through a drip into a vein (IV infusion). They are usually combined with chemotherapy and are commonly given in repeating cycles. Talk to your doctor about your specific treatment schedule.
Side effects of monoclonal antibody therapy
Your doctor will let you know of potential side effects before you start treatment. Side effects can include headache, fatigue, anaemia, flu-like symptoms and an increased risk of abnormal bleeding. You will have regular check-ups during treatment.
Some people react to the infusion process (e.g. nausea, skin rashes and itching) during treatment or several hours after the infusion. Reactions are more common with the first infusion, with the risk declining after every dose. You may be given medicine to help prevent such a reaction.
In some people, rituximab can reactivate some viral infections, such as hepatitis B. It can also increase your risk of getting another infection. It is important to discuss any side effects with your doctor immediately. If left untreated, some symptoms can become life-threatening.
For more on this, see our general sections on Targeted therapy and Immunotherapy.
Small molecule inhibitors
Small molecule inhibitors are another type of targeted therapy. These drugs can get inside cancer cells and block certain proteins that tell the cancer cells to grow.
Small molecule inhibitors (such as acalabrutinib, ibrutinib, idelalisib and zanubrutinib) are used to treat some types of low-grade lymphoma that have not responded to treatment or have come back. In some cases, small molecule inhibitors may also be an option if you are older.
Talk with your doctor about whether these treatments (or another drug available on a clinical trial) are suitable for your situation.
These drugs have the potential to cause a variety of side effects – your doctor will discuss these with you before you start treatment.
Video: What is targeted therapy?
Watch this short video to learn more about targeted and immunotherapy.
Podcast: Immunotherapy & Targeted Therapy
Listen to more episodes from our podcast for people affected by cancer
More resources
Dr Puja Bhattacharyya, Haematology Staff Specialist, Western Sydney Local Health District, Blacktown Hospital; A/Prof Christina Brown, Haematologist, Royal Prince Alfred Hospital and The University of Sydney; Dr Susan Carroll, Senior Staff Specialist, Radiation Oncology, Royal North Shore Hospital and The University of Sydney; Jo Cryer, Clinical Nurse Consultant, Haematology, St George Hospital; Marie Marr, Consumer; Katelin Mayer, Clinical Nurse Consultant, Cancer Outreach Team, Nelune Comprehensive Cancer Centre, Sydney; Vanessa Saunders, 13 11 20 Consultant, Cancer Council NSW; Elise Toyer, Haematology Clinical Nurse Consultant, Blacktown Hospital.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.