- Home
- Ovarian cancer
- Treatment
- Surgery
Surgery for ovarian cancer
Surgery is often the initial treatment for ovarian cancer. This surgery can be complex. It is recommended that a gynaecological oncologist who is at a hospital that does a lot of these operations (a high-volume centre) does the surgery.
The Australian Society of Gynaecologic Oncologists has a list of specialists by state and territory. Visit asgo.net.au/is-there-a-gynaecologist-oncologist-near-you, to find a specialist near you.
Learn more about:
- Overview
- How the surgery is done
- Having a surgical biopsy
- Debulking
- Types of surgery
- What to expect after surgery
- Taking care of yourself at home after surgery
Overview
Surgery allows your gynaecological oncologist to confirm the diagnosis of ovarian cancer and also work out if the cancer has spread.
The gynaecological oncologist will talk to you about the most suitable type of surgery, as well as the risks and side effects. These may include infertility. If the option to have children is important to you, talk to your doctor before surgery and ask for a referral to a fertility specialist.
For more on this, see our general section on Surgery.
How the surgery is done
You will be given a general anaesthetic and will have either a laparoscopy (with 3–4 small cuts in your abdomen) or a laparotomy (with a vertical cut from around your bellybutton to your pubic line). A laparoscopy may be used to see if a suspicious mass is cancerous; if the cancer is advanced, you will usually have a laparotomy.
Having a surgical biopsy
You may have a biopsy during surgery if you cannot have an image-guided biopsy, or to remove and check a suspicious tumour. The tissue samples will be sent to a pathologist, who will check them for signs of cancer. The results will help decide if you need debulking surgery (see below).
Debulking
If cancer is found, the surgeon will remove as much visible cancer as possible. This is called debulking or cytoreductive surgery. You may also have chemotherapy before or after surgery.
Debulking usually means removing the ovaries, fallopian tubes, uterus and cervix. Depending on how far the cancer has spread, other organs or tissue may also be removed during the same operation.
| Omentectomy | The omentum is a sheet of fatty tissue that hangs down in front of the large bowel like an apron. If the cancer has spread to the omentum, it will need to be removed. The omentum may also be removed even if there is no visible sign cancer has spread, because it may contain cancer cells that cannot be seen during surgery. |
| Lymphadenectomy | Cancer cells can spread from your ovaries to nearby lymph nodes. Your doctor may suggest removing some nodes in a lymphadenectomy (also called lymph node dissection). |
| Colectomy | If cancer has spread to the bowel, some of the bowel may need to be removed. Rarely, a new opening called a stoma might be created (colostomy or ileostomy). |
| Removal of other organs | Ovarian cancer can spread to many organs in the abdomen. In some cases, parts of the liver, diaphragm, bladder and spleen may be removed if it is safe to do so. |
Types of surgery
If ovarian cancer is found, all or some of the reproductive organs will be removed. The type of surgery you have will depend on how certain the gynaecological oncologist is that cancer is present and where the cancer has spread.
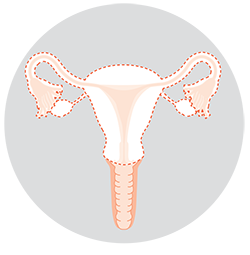 | Total hysterectomy and bilateral salpingo-oopherectomyIn most cases, surgery for ovarian cancer means removing the uterus and cervix, along with both fallopian tubes and ovaries.Removing the uterus will mean you cannot get pregnant and carry a child. |
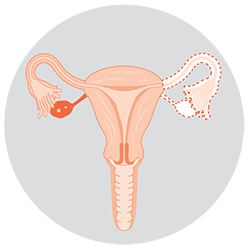 | Unilateral salpingo-oophorectomyIf cancer is found early and it is in one ovary, you may have only one ovary and fallopian tube removed.This may be offered to some younger women with early-stage cancer who still wish to have children. |
I felt great relief after the surgery, as once the tumour had been removed, the pain that I had in my lower abdomen and hip was gone.
Ann
→ READ MORE: What to expect after surgery
Podcast: Making Treatment Decisions
Listen to more episodes from our podcast for people affected by cancer
More resources
Dr Antonia Jones, Gynaecological Oncologist, The Royal Women’s Hospital and Mercy Hospital for Women, VIC; Dr George Au-Yeung, Medical Oncologist, Peter MacCallum Centre, VIC; Dr David Chang, Radiation Oncologist, Peter MacCallum Cancer Centre, VIC; Prof Anna DeFazio AM, Sydney West Chair of Translational Cancer Research, The University of Sydney, Director, Centre for Cancer Research, The Westmead Institute for Medical Research and Director, Sydney Cancer Partners, NSW; Ian Dennis. Consumer (Carer); A/Prof Simon Hyde, Head of Gynaecological Oncology, Mercy Hospital for Women, VIC; Carmel McCarthy, Consumer; Quintina Reyes, Clinical Nurse Consultant – Gynaecological Oncology, Westmead Hospital, NSW; Deb Roffe, 13 11 20 Consultant, Cancer Council SA.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.

