- Home
- Soft tissue sarcoma
- Treatment
Soft tissue sarcoma treatment
In this section, we discuss the different treatment options available for someone diagnosed with soft tissue sarcoma.
Learn more about:
- Making decisions about treatment
- Your treatment options
- Surgery
- Radiation therapy
- Chemotherapy
- Targeted therapy
- Joining a clinical trial
- Involvement in research
- Complementary therapies and integrative oncology
- Side effects of treatment
- Nutrition and exercise
Making decisions about treatment
It can be difficult to know which treatment is best for you. It is important that you speak with a sarcoma specialist team before making your decisions. Ask them to give you a plan of your treatment options, as well as information about side effects. If you are confused or want to check anything, ask questions. This will make sure you have all the information you need to make decisions about treatment and your future that you are comfortable with.
Some people prefer to seek several opinions before feeling confident to go ahead with the treatment. It is important to seek second opinions from a sarcoma specialist; these are listed on the Australia and New Zealand Sarcoma Association (ANZSA) find a sarcoma specialist directory and Rare Cancers Australia knowledgebase directory.
You may have to attend many appointments. It’s a good idea to take a family member or friend with you so they will be able to listen, ask questions and remember what the doctor says.
It may help to take a list of questions with you, take notes (especially about anything you are unfamiliar with) or ask the doctor if you can record the discussion (many mobile phones have a recording function or you can use the CAN.recall app – visit rarecancers.org.au for more information). Here are some suggestions for questions you could ask.
Your treatment options
You will be cared for by a multidisciplinary team (MDT) of health professionals during your treatment for soft tissue sarcoma. The team may include a surgeon, radiation oncologist (to prescribe and coordinate a course of radiation therapy), medical oncologist (to prescribe and coordinate a course of systemic therapy which includes chemotherapy), paediatric oncologist, nurse and allied health professionals such as a dietitian, social worker, psychologist or counsellor, physiotherapist and occupational therapist.
Discussion with your doctor will help you decide on the best treatment for your sarcoma depending on:
- the type of sarcoma you have
- where it is in your body
- whether or not the cancer has spread (stage of disease)
- your age, fitness and general health
- your preferences.
The main treatments include surgery, chemotherapy and radiation therapy. These can be given alone or in combination. This is called multi-modality treatment.
For an overview of what to expect during all stages of your cancer care, visit Sarcoma (Bone and soft tissue tumours) – Your guide to best cancer care. This is a short guide to what is recommended, from diagnosis to treatment and beyond.
Surgery
Surgery is the main treatment for most types of soft tissue sarcoma. Surgery usually involves removing the cancer and some healthy tissue around the cancer. This is called a wide local excision. The healthy tissue is removed to help reduce the risk of the cancer coming back in that area.
The type of operation depends on where the sarcoma is. Most sarcomas are in the arm or leg. This usually means having limb-sparing surgery; amputation is less common. If the sarcoma is in another part of the body, for example the chest or abdomen, surgery will depend on where the cancer is and how big it is. Your surgeon will discuss the type of operation you may need.
The most important thing is that you have your surgery done by an experienced surgeon working in a specialist centre for sarcoma.
For more on this, see our general section on Surgery or call 13 11 20.
Support programs
If you need major surgery like amputation, you may find it helps to speak with a social worker or counsellor. You might also find it beneficial to talk to others who have been through a similar experience.
Cancer Council offer a range of support programs including telephone, online, and peer to peer support groups. Call 13 11 20 and speak to a cancer health professional about what might suit you best.
Radiation therapy
Radiation therapy (also known as radiotherapy) uses high energy rays to destroy cancer cells. Sarcoma is known to be very sensitive to radiation therapy.
It may be used:
- before surgery, to destroy the cancer cells and create a ‘rind’ around the cancer, which helps the surgeon to perform good surgery
- if the cancer is too big to remove with surgery
- if the cancer has spread to other parts of the body
- after surgery, to destroy any remaining cancer cells and stop the cancer coming back
- if the cancer is in a place in the body that is too hard to reach using surgery.
Radiation therapy can shrink the cancer down to a smaller size. This may help to make surgery easier. Sometimes chemotherapy is given as well as radiation therapy, to help make the treatment more effective. This depends on the type of sarcoma.
A course of radiation therapy needs to be carefully planned. During your first consultation session you will meet with a radiation oncologist who will arrange a planning session. At the planning session (known as CT planning or simulation) you will need to lie still on an examination table and have a CT scan in the same position you will be placed in for treatment.
The information from the planning session will be used by your specialist to work out the treatment area and how to deliver the right dose of radiation. Radiation therapists will then deliver the course of radiation therapy as set out in the treatment plan.
Radiation therapy does not hurt and is usually given in small doses over a period of time to minimise side effects.
For more on this, see our general section on Radiation therapy or call 13 11 20.
Chemotherapy
Chemotherapy (sometimes just called “chemo”) is the use of drugs to kill or slow the growth of cancer cells. You may have one chemotherapy drug, or a combination of drugs. This is because different drugs can destroy or shrink cancer cells in different ways.
Your treatment will depend on your situation and the type of sarcoma you have. It may also be used to help stop a sarcoma coming back after surgery. Your medical oncologist will discuss options with you.
Most often chemotherapy is given through a drip into a vein (intravenously) or as a tablet that is swallowed. It can also be given as a cream or as injections into different parts of the body. Having a needle inserted for intravenous chemotherapy feels like having blood taken. If you have a temporary tube (cannula) in your hand or arm only the initial injection may be uncomfortable. Your medical oncologist may recommend a central venous access device (also known as a ‘central line’). This is put into a vein in your neck or chest under local or general anaesthetic and stays in throughout your treatment so you don’t have to have lots of needles. You can also have your blood taken from this line.
Chemotherapy is commonly given in treatment cycles which may be daily, weekly or monthly. For example, one cycle may last three weeks where you have the drug over a few hours, followed by a rest period before starting another cycle. The length of the cycle and number of cycles depends on the chemotherapy drugs being given.
For more on this, see our general section on Chemotherapy.
Targeted therapy
Targeted therapy is a cancer treatment that uses drugs to target specific genes and proteins that are involved in the growth and survival of cancer cells. It uses drugs that work in a different way to chemotherapy drugs.
While chemotherapy affects all rapidly dividing cells and works by killing cancerous cells (cytotoxic), targeted therapy attacks specific molecules within cells and often works by blocking cell growth (cytostatic). People with soft tissue sarcomas may be offered targeted therapies such as pazopanib (Votrient) to slow the growth of the tumour.
For more on this, see our general section on Targeted therapy.
Clinical trials
Your doctor or nurse may suggest you take part in a clinical trial. Doctors run clinical trials to test new or modified treatments and ways of diagnosing disease to see if they are better than current methods.
For example, if you join a randomised trial for a new treatment, you will be chosen at random to receive either the best existing treatment or the modified new treatment. Over the years, trials have improved treatments and led to better outcomes for people diagnosed with cancer.
You may find it helpful to talk to your specialist, clinical trials nurse or GP, or to get a second opinion. If you decide to take part in a clinical trial, you can withdraw at any time.
For more information, visit Australian Cancer Trials and the Australia and New Zealand Sarcoma Association (ANZSA).
For information on gastro-intestinal stromal sarcoma (GIST) clinical trials visit the Australasian Gastro-Intestinal Trials Group (AGITG).
For more on this, see our general section on Clinical trials and research or call 13 11 20.
Involvement in research
You may wish to be involved in research in addition to clinical trials, or perhaps because you and your doctor can’t find a clinical trial suitable for your needs. Some research studies enable your cancer to be studied in more detail in the laboratory.
These studies will require samples of your cancer tissue and other tissues, such as your blood, and your clinical data to be collected. You would need to read a patient information and consent form to decide whether you wish to take part in this kind of research prior to providing your consent.
Information about these types of research studies may be available at your treatment centre or from websites such as the Australian New Zealand Clinical Trials Registry which lists appropriate studies.
For more information, visit:
- Australian and New Zealand Clinical Trials Registry
- Australia and New Zealand Sarcoma Association
- The International Sarcoma Kindred Study
- Genetic Cancer Risk in the Young (RisC) Study
- The Molecular Screening and Therapeutics (MoST) Study.
Complementary therapies and integrative oncology
Complementary therapies are designed to be used alongside conventional medical treatments (such as surgery, radiation therapy and chemotherapy) and can increase your sense of control, decrease stress and anxiety, and improve your mood. Some Australian cancer centres have developed “integrative oncology” services where evidence-based complementary therapies are combined with conventional treatments to improve both wellbeing and clinical outcomes.
Let your doctor know about any therapies you are using or thinking about trying, as some may not be safe or evidence-based.
Complementary therapy | Clinically proven benefits |
| acupuncture | reduces chemotherapy-induced nausea and vomiting |
| aromatherapy | improves sleep and quality of life |
| art therapy, music therapy | reduce anxiety and stress; manage fatigue; aid expression of feelings |
| counselling, support groups | help reduce distress, anxiety and depression; improve quality of life |
| hypnotherapy | reduces pain, anxiety, nausea and vomiting |
| massage | improves quality of life; reduces anxiety, depression, pain and nausea |
| meditation, relaxation, mindfulness | reduce stress and anxiety; improve coping and quality of life |
| qi gong | reduces anxiety and fatigue; improves quality of life |
| spiritual practices | help reduce stress; instil peace; improve ability to manage challenges |
| tai chi | reduces anxiety and stress; improves strength, flexibility and quality of life |
| yoga | reduces anxiety and stress; improves general wellbeing and quality of life |
Alternative therapies are therapies used instead of conventional medical treatments. These are unlikely to be scientifically tested and may prevent successful treatment of the cancer. Cancer Council does not recommend the use of alternative therapies as a cancer treatment.
For more on this, see our general section on Complementary therapies.
Side effects of treatment
All treatments can have side effects. The type of side effects that you may have will depend on the type of treatment and where in your body the cancer is. Some people have very few side effects and others have more. Your specialist team will discuss all possible side effects, both short-term and long-term (including those that have a late effect and may not start immediately), with you before your treatment begins. One issue that is important to discuss before you undergo treatment is fertility, particularly if you want to have children in the future.
For more on this, see Fertility and cancer or call 13 11 20.
Common side effects
| Surgery | Nausea and vomiting from the anaesthetic, bleeding, damage to nearby tissue and organs (including nerves), drug reactions, pain, infection after surgery, blood clots, weak muscles (atrophy), lymphoedema |
| Radiation therapy | Fatigue, loss of appetite, nausea, bowel issues (such as diarrhoea, abdominal cramps and excess wind), bladder issues, hair loss, dry mouth, skin problems, lymphoedema, loss of fertility, early menopause |
| Chemotherapy | Fatigue, loss of appetite, nausea, bowel issues (such as constipation or diarrhoea), hair loss, mouth sores, skin and nail problems, increased chance of infections, loss of fertility, early menopause |
Nutrition and exercise
If you have been diagnosed with soft tissue sarcoma, both the cancer and treatment will place extra demands on your body. Research suggests that eating well and exercising can greatly benefit people both during and after cancer treatment. Eating well and being active can help you cope with some of the common side effects of cancer treatment, speed up recovery, improve sleep, and help improve quality of life by giving you more energy, keeping your muscles strong, helping you maintain a healthy body weight and boosting your mood.
You can discuss individual nutrition and exercise plans with health professionals such as dietitians, exercise physiologists and physiotherapists.
For more on this, see Nutrition and cancer and Exercise for people living with cancer or call 13 11 20.
→ READ MORE: Life after treatment
Podcast: Making Treatment Decisions
Listen to more episodes from our podcast for people affected by cancer
More resources
Dr Susie Bae, Medical Oncologist, Peter MacCallum Cancer Centre, VIC; Tony Bice, Consumer; Dr Denise Caruso, CEO Australian and New Zealand Sarcoma Association, VIC; Emma Gardner, Nurse Coordinator, Bone and Soft Tissue Unit, Peter MacCallum Cancer Centre, VIC; Jonathan Granek, Consumer; Thelma Lobb, Consumer.
View the Cancer Council NSW editorial policy.
Need to talk?
Support services
Coping with cancer?
Speak to a health professional or to someone who has been there, or find a support group or forum
Need legal and financial assistance?
Pro bono services, financial and legal assistance, and no interest loans
Cancer information
What is cancer?
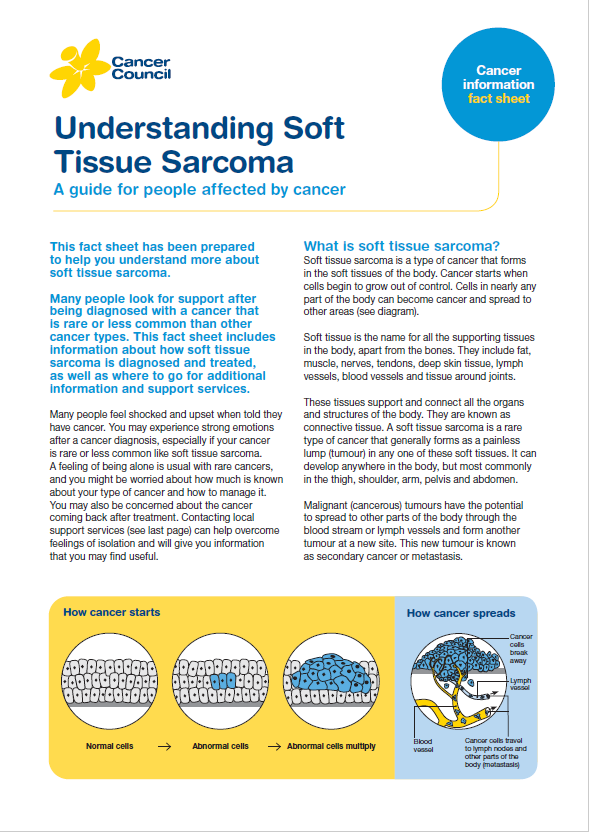
How cancer starts and spreads
Resource hub
Guides, fact sheets, videos, podcasts and more for people with cancer, their families and friends