- Home
- Cancer of the uterus
- Managing side effects
- Lymphoedema and cellulitis
Lymphoedema and cellulitis
After surgery or radiation therapy to the pelvic area, you may find that one or both legs become swollen. This is known as lymphoedema. Another possible side effect after lymph node removal is a skin infection known as cellulitis.
Learn more about:
Lymphoedema
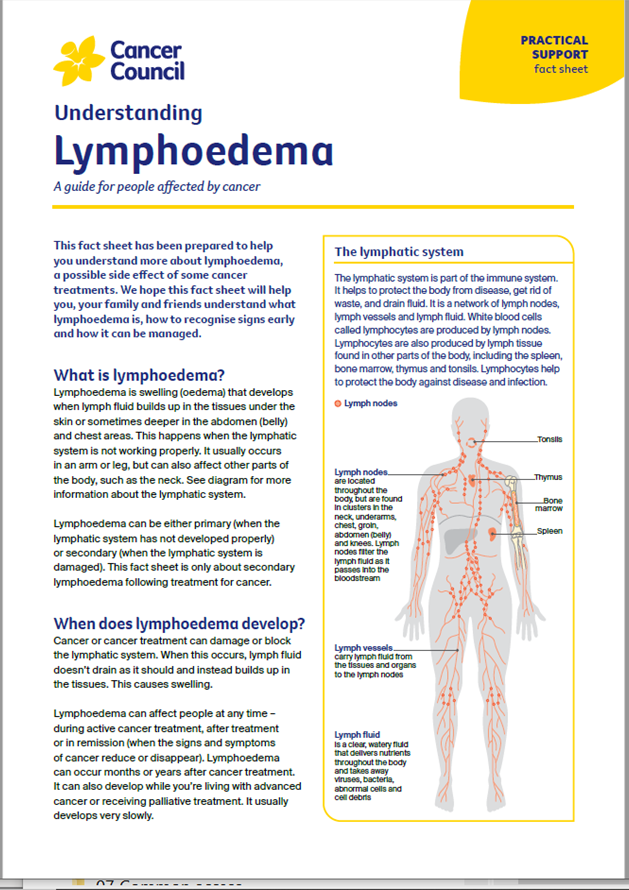
Lymphoedema occurs when lymph fluid doesn’t circulate properly and builds up. The swelling may appear during treatment or months or years later.
Lymphoedema can make movement and some types of activities difficult. It is important to maintain a healthy body weight, avoid pressure, injury or infection to the legs, and manage lymphoedema symptoms as soon as possible.
Mild lymphoedema is usually managed with exercise, skin care and a compression stocking. To find a health professional who specialises in the management of lymphoedema, speak to your treatment team or visit the Australasian Lymphology Association.
Learn more about lymphoedema.
If your GP refers you to an allied health professional (such as a physiotherapist) as part of a chronic disease management plan, you may be eligible for a Medicare rebate for up to five visits each year. Ask your GP for more details.
Cellulitis
The skin on the legs may become infected more easily after lymph nodes are removed. A common skin infection is called cellulitis. Signs of cellulitis include redness, painful swelling, warm skin and fever. If you have any symptoms, see your GP as soon as possible.
To reduce the risk of infection, keep the skin healthy and unbroken, exercise regularly and avoid tight-fitting clothing. Use moisturiser and sunscreen, and avoid scratches, cuts, burns, insect bites, and injections in your legs. Also, keep your feet clean and dry to avoid fungal infections.
→ READ MORE: Vaginal narrowing and dryness
Podcast: Managing Cancer Pain
Listen to more episodes from our podcast for people affected by cancer
More resources
A/Prof Orla McNally, Consultant Gynaecological Oncologist, Director Oncology/Dysplasia, Royal Women’s Hospital, Honorary Clinical Associate Professor, University of Melbourne, and Director of Gynaecology Tumour Stream, Victorian Comprehensive Cancer Centre, VIC; A/Prof Yoland Antill, Medical Oncologist, Peninsula Health, Parkville Familial Cancer Centre, Cabrini Health and Monash University, VIC; Grace Guerzoni, Consumer; Zeina Hayes, 13 11 20 Consultant, Cancer Council Victoria; Bronwyn Jennings, Gynaecology Oncology Clinical Nurse Consultant, Mater Hospital Brisbane, QLD; A/Prof Christopher Milross, Director of Mission and Radiation Oncologist, Chris O’Brien Lifehouse, NSW; Mariad O’Gorman, Clinical Psychologist, Liverpool Cancer Therapy Centre and Bankstown Cancer Centre, NSW.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.
Need to talk?
Support services
Life after cancer treatment
Programs and support for people who have finished treatment
Support post treatment
Support and information for cancer survivors
Cancer information
Nutrition and cancer
How to eat well during and after cancer treatment
Staying healthy after treatment
Lifestyle changes that can help keep you in good health